
Medical
Communication
Biosci. Biotech. Res. Comm. 10(2): 40-48 (2017)
Evaluation of tissue dissolution ability of modi ed
chlorhexidine as a root canal irrigant
Samira Shahsiah
1
, Arash Azizi
2
*, Eskandar Moghimipour
3
, Paul V. Abbott
4
,
Kasra Karamifar
5
, Mansour Jafarzadeh
6
and Mina Fazeli
7
1
Department of Endodontics, Faculty of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2
Oral medicine Department, Islamic Azad University,Dental Branch, Tehran, Iran
3
Medicinal Plant Research Center,Faculty of Pharmacy,Ahvaz Jundishapur University of Medical Sciences,
Ahvaz, Iran
4
Winthrop Professor of Clinical Dentistry,University of Western Australia, Australia
5
Department of Endodontics, Dental Branch, Shiraz Islamic Azad University, Shiraz, Iran
6
Department of Endodontics, Faculty of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
7
Dentist
ABSTRACT
The rst and main goal of root canal treatment is the elimination of microorganisms from the contaminated root canal system
and providing an environment for the healing of periapical tissues. Instrumentation alone cannoteffectivelyclean the complex
root canal system. Souse of irrigantsalong mechanicalpreparationis required. But no single solution is able to ful ll these actions
completely. Chlorhexidineis one of the substances thatis usedas anirrigantin endodontics. It has broadantimicrobialspectrum, but
itdoes not have theability todissolveorganictissues. It has been shownthat theaddition ofsurfactantin thesolution can increasesthe
abilityof dissolvetissue.In this in vitro study tissue-dissolving capacity of sodium hypochlorite (5/25% and 2/5%), chlorhexidine
(0/2%) and modi ed chlorhexidine (chlorhexidine + benzalkonium chloride and chlorhexidine + sodium lauryl solphate) were
compared.Tissue samples prepared from bovine pulp and each of the samples immersed for 20 minutes in each test solution
(changing the solution every 2 minutes).The sampleswereweighedbefore and aftertesting. The weight difference divided by the
initial weight of the tissue sample, multiplied by 100, was de ned as the percentage of tissue solubility.NaOCl 5/25% was more
solublethantheothersolutions. ExceptCHX 0/2% and salineno statistically signi cant differences was found between the tissue-
dissolving properties of othersolutions and NaOCl 5/25%.The results of this study indicate that the use of 0/2%CHX+2%SLS as
irrigant in endodontic can show similar effect with NaOCl 5/25% in the solubility.
KEY WORDS: ROOT CANAL THERAPY, CHLORHEXIDINE, TISSUE SOLABILITY, BENZALKONIUM CHLORIDE, SODIUM LAURYL SULPHATE
40
ARTICLE INFORMATION:
*Corresponding Author: drarashazizi@yahoo.com
Received 12
th
April, 2017
Accepted after revision 30
th
June, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF : 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at: http//www.bbrc.in/
Samira Shahsiah et al.
INTRODUCTION
Studies illustrated that different methods of using tools
during cleaning and forming produces smear layer
which covers dentinaltubule canal and inlet (Johnson
W.T , et al, 2008; Belts R.E , et al, 2003). This layer diam-
eter is mμ2- and it is disordered and formless (Karale R
, et al, 2011). From Pulp organic ingredients and inor-
ganic dentin debri, micro-organisms, their products and
necrotic are formed (Johnson W.T , et al, 2008; Karale R ,
et al, 2011; Baumgartner J.C , et al, 2007; Belts R.E , et al,
2003). Smear layer presence avoids penetration of medi-
cine in canal into root canal system and dentinal tubules
and also prevents full compatibility of lling materials
with surface of canal prepared walls (Belts et al, 2003).
Different acids, ultra sonic tools, and lasers are used
for removing this layer (Belts et al, 2003). One material is
Ethylene diaminete traacetic acid (EDTA). This chemical
is part of chelatorthat has capacity of removing inor-
ganic elements however cannot remove inorganic mate-
rials. So there is need to use a tissue solvent material
such as NaOCl. Recommended time for removing smear
layer by EDTA is 1 minute. This material will cause pre-
tubular and intratubular exceeding omission (Johnson et
al, 2008). Generally, detergents are categorized as follow
(Kandaswamy and Venkateshbabu 2010):
Sodium hypochlorite (NaOCl) with density of 5/0–
25/5% is the most prevalent detergent which is used for
endodontic treatments (Karale et al, 2011; Guerreiro-
Tanomaru 2011). NaOCl has different advantages includ-
ing mechanical cleaning of debris of canal, capacity of
solving alive tissues and necrotic, anti-microbial activ-
ity, blundering activity and long shelf-life. In addition,
this cheap material is highly accessible (Johnson et al,
2008; Karale et al, 2011; Guerreiro-Tanomaru 2011).
Popular density of NaOCl is 5/2%in which tissue solu-
bility and anti-microbial characteristics are maintained.
This density normally is used in teeth with necrotic pulp
or apical priodentit (Johnson et al, 2008; Guerreiro-
Tanomaru 2011).
NaOCl averagely is effective against bacteria but
it has less effect against endotoxin in infected canals
(Kandaswamy and Venkateshbabu 2010). It has also
some restrictions in solving tissues due to limited con-
tact with existing tissues in whole canal space (Johnson
et al, 2008).Unfortunately using NaOCl has some disad-
vantage. This material is very toxic and creates severe
in ammatory reaction in addition when it crosses the
root apex accidentally; it produces severe pain, swelling
and hematoma (Karale et al, 2011).
Chlorhexidine gluconate (CHX) is a mouth wash that
is used in different densities as a detergent for endo-
dontic treatment. CHX is a broad extent anti-microbial
factor against gram-positive bacteria and gram-negative
bacteria. This material has low toxic property and it is
absorbed by dental tissue and mucousmembrane, while
its effective material is released slowly. Biocompatibility
property and substantivity of CHX justi es clinical use
of this material (Kandaswamy and Venkateshbabu 2010;
Karale 2011; Guerreiro-Tanomaru 2011). Anti-microbial
property of 2% CHX is similar to NaOCl 25/5% while
enterococcus faecalis is more effective (Johnson et al,
2008). One disadvantage of Chlorhexidine gluconate is
lack of ability for solving necrotic tissue and remov-
ing smear-layer (Johnson et al, 2008; Kandaswamy and
Venkateshbabu 2010) which may has effect on other
properties of this material (Guerreiro-Tanomaru J.M,
2011).
Out of different materials, surfactant had accept-
able solubility, because it has either Hydro philic or
hydrophobe properties. This material is solved in hydro
phase through hydrophilic property and it is solved via
hydrophobo in organic phase and cause solution of
present material in both phases. In addition, this mate-
FIGURE 1. Endodontic detergents
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE 41

Samira Shahsiah et al.
rial decreases surface tension of bacteria cell walls so
it destroys them via which it implements anti-bacterial
properties (Aulton and Taylor 2008).
According to disadvantage of NaOCl including toxic-
ity and providing sever in ammatory reactions (Karale
et al, 2011 ) and based on advantages of CHX including
broad antimicrobial property, informality and biocom-
patibility, using CHX as detergent is more appropriate
in endodontic treatment. However lack of ability of this
material in solubility of remained tissues has caused
limitation of its application. So adding one material
with tissue solubility properties into CHX can handle
this problem and it can provide a detergent with better
properties.
Irrigation of root canal during root treatment is an
important phase. There is no evidence that approved
detergent type role in success of the treatment. So there
is no agreement on what detergent is the best one or on
what detergents are better if they are both used. How-
ever they all agree that the detergent need to have anti-
microbial activity. The best result is obtained from using
a good detergent with anti-bacterial activity when it
contacts long enough with batteries of root canal system.
This means that, for ful lling preparation stage before
obtuaration, detergent needs to be reached a suf cient
volume during the treatment (Iqbal 2012). It seems that
using local medicine is more effective and better that all
applicable antibiotic plans (Martin 1991).
Irala et al (2010) in Luterana University in Brazil per-
formed studies on different densities on NaOCl alone
and also with combination of EDTA. Results indicated
that combination of NaOCl with EDTA has no ability of
tissue solution. T-test also indicated that 2/5% NaOCl
solve the tissue in less time than 1% NaOCl. On the
other hand, solutions’ PH were decreased in 48 hours. In
addition, Cobankara et al in 2010 in Secuk univesristy
of Turkey performed an experiment on Cobankara and
chlorine dioxide. Studies illustrated that saline has no
capacity of solving organic tissue. Both 25/5% NaOCl
and 8/13%ClO
2
solution more effectively solved pulp tis-
sue in compare to control saline (P<0/05). On the other
hand, no statistical difference between solubility capac-
ity of 25/5% NaOCl and 8/13%ClO
2
was observed. It was
indicated that both materials have similar effect con-
sidering tissue solubility. In addition, Cbristensen et al
(2008) in Alabama Birmingham University investigated
effect of sodium hypochlorite PH decrease on its tis-
sue solubility property. Statistical results did not show
signi cant difference in groups with PH 12 and PH9.
While there was signi cant difference in groups with PH
12 and PH 9 and group with PH6. Higher densities and
longer durations caused increase of solubility.
In this study two surfactantincluding 4% Benzalko-
nium and 2% Sodium lauryl Sulfate have been studied.
General objective is study of tissue solubility of changed
chlorhexidinein root cleaning. We aimed at answering
following questions:
– How much is the weight loss percentage of pulp
tissue after using 5.25%NaOCl solution?
– How much is the weight loss percentage of pulp
tissue after using 2.5%NaOCl solution?
– How much is the weight loss percentage of pulp
tissue after using 0.2% CHX solution?
– How much is the weight loss percentage of pulp
tissue after using CHX + Benzalkonium chloride
solution?
– How much is the weight loss percentage of pulp
tissue after using CHX + Sodium lauryl sulfate
solution?
– Are weight loss percentages of pulp tissue differ-
ent in experimental groups?
At the following we explained materials and methods
of collecting data and collecting samples. In section 3
we provided research results and statistical tests. After
discussing the cases we provided nal conclusion.
MATERIALS AND METHODS
In this study, in order to providing pulp samples, we used
bovine mandible of one-year-old calf from slaughter-
house. Milkanseizure teeth were separated from mandi-
ble. There was germ on permanent anseizure tooth under
these teeth which was accessible by mandible bone
cleavage. Teeth pulp covered with thin skin of enamel
was separated and It was kept in 40-c degree in central
laboratory of Pharmacy department until experiment’s
time. Solutions of the experiment were prepared by an
expert from laboratory of Pharmacy department who
had no interference in. and he coded them from number
1 to 6. The tester had no information of group codes
and solution types. Solution lists are as follow:NaOCl
25/5%,NaOCl 5/2%,benzalkonium chloride 4% CHX
+2/0%, sodium lauryl sulfate2% CHX +2/0%, CHX
2/0%,NaCl9/0% as a controller
During experiment, pulp samples were divided into
sections with weight approximate to 25mg. samples were
categorized in 5 groups with 10 samples and one group
with 5 samples as control group.Each sample weight
was measured with digital scale before experiment.
Sample was transferred to experiment tube and tube
were coded. After preparation of samples, 2ml experi-
ment solution was poured on pulp sample in experiment
tube by syringe. And sample was place on vibrator for 2
minutes. After 2 minutes the solution was extracted by
syringe from experiment tube. Then 2ml fresh solution
was added to the sample and it was placed on vibrator
for another two minutes. This process was performed for
42 EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Samira Shahsiah et al.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE 43
10 times for each sample. By this method, each sample
had contact with fresh solution for 20 minutes. After 20
minutes, all solution was extracted by syringe from the
tube and pulp sample was dried. Finally, weight of dry
pulp sample was measured by the same digital scale and
it was recorded.
This method was performed for each 6 group and
the results were recorder. For calculating percentage of
weight loss, weight difference of tissue sample before
and after contact with solution under experiment was
divided into initial weight of tissue and was multiplied
in 100 (Zehnder M, 2006; Siqueira J.F, et al, 2009). In
order to test obtain results, data summary was reported
for average and standard deviation of X±SD and in
order to comparing groups we used one-way analysis
and then we used post hoc for pairwise.
Based on before studies, there would be 10 samples
in each group with 25ml weight (Kleier et al, 2008). In
this study, 6 groups of solution were experimented. Tis-
sue samples were washed with solutions. For calculat-
ing percentage of weight loss, weight difference of tis-
sue sample before and after contact with solution under
experiment was divided into initial weight of tissue and
was multiplied in 100. Results are in table (1).
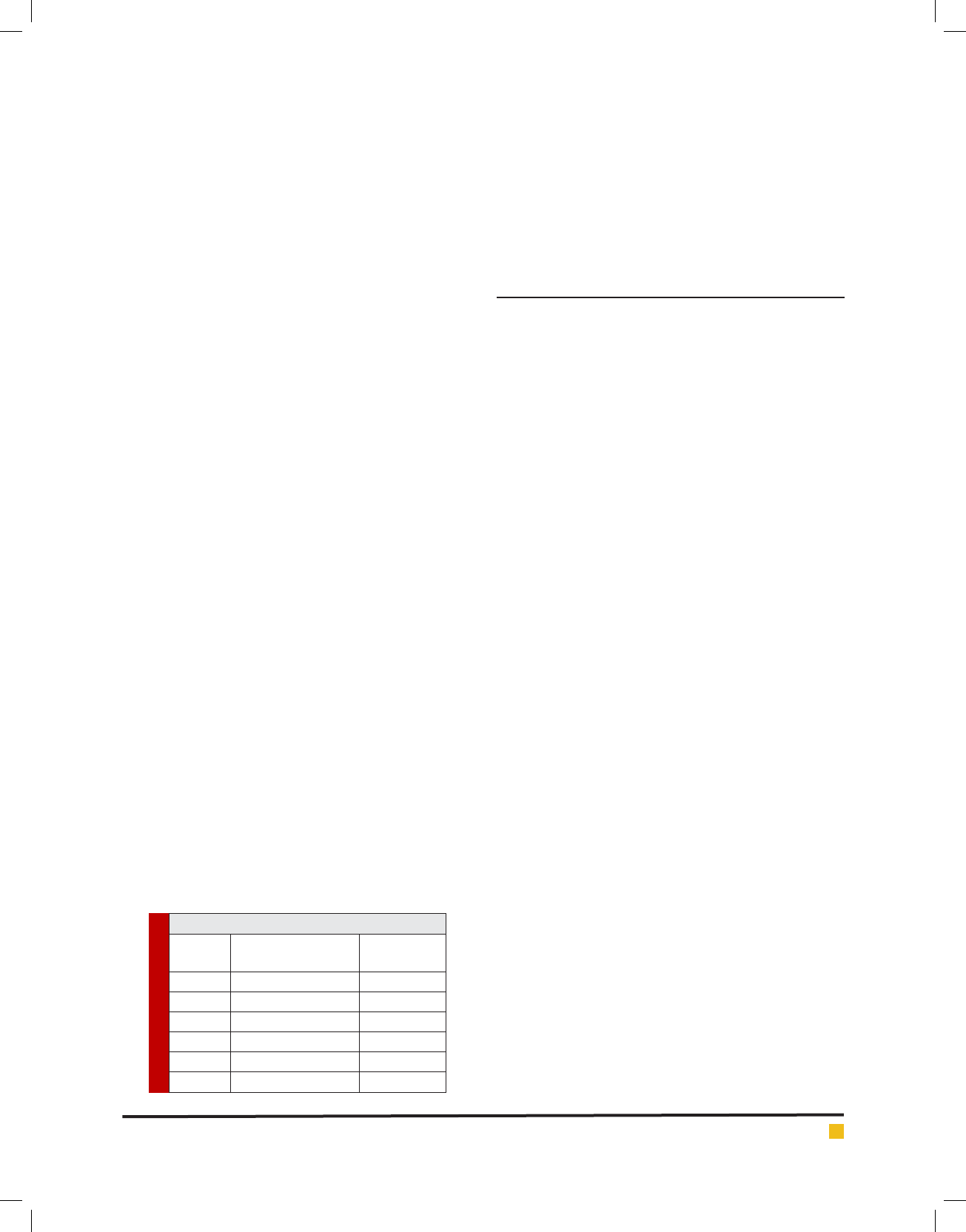
In addition, diagrams (1) to (6) represent percentage
of tissue solubility in samples of group 1 to 6. Solu-
tion with code number 1 which included 25/5%sodium
hypochlorite averagely indicated solubility percentage
as 70/53%. In this group, 6 samples show solubility per-
centage above 50% and 4 sample showed solubility per-
centage below 40%.
Solution with code number 2 included 2/5% sodium
hypochlorite. Tissue solubility had 07/27% average while
out of 10 samples one sample showed 50% solubility,
one sample showed negative solubility and other sam-
ples showed solubility under 50%.. solution number 3
included chlorhexidine+ benzalkoniumchloride showed
average of 39/32% tissue solubility and out of all sample
one sample showed solubility above 50% and other sam-
ples showed solubility below 50%. In addition, solution
number 4 included chlorhexidine+ 2% sodium dodecyl
sulfates showed solubility average as 83/34% while all
10 samples showed solubility below 40%. However solu-
tion number 6 included normal saline which was used
as control solution and showed average 66/0- %tissue
solubility. Out of 5 samples under study, 2 samples had
solubility below 10%, one sample zero solubility and 2
samples showed negative solubility.
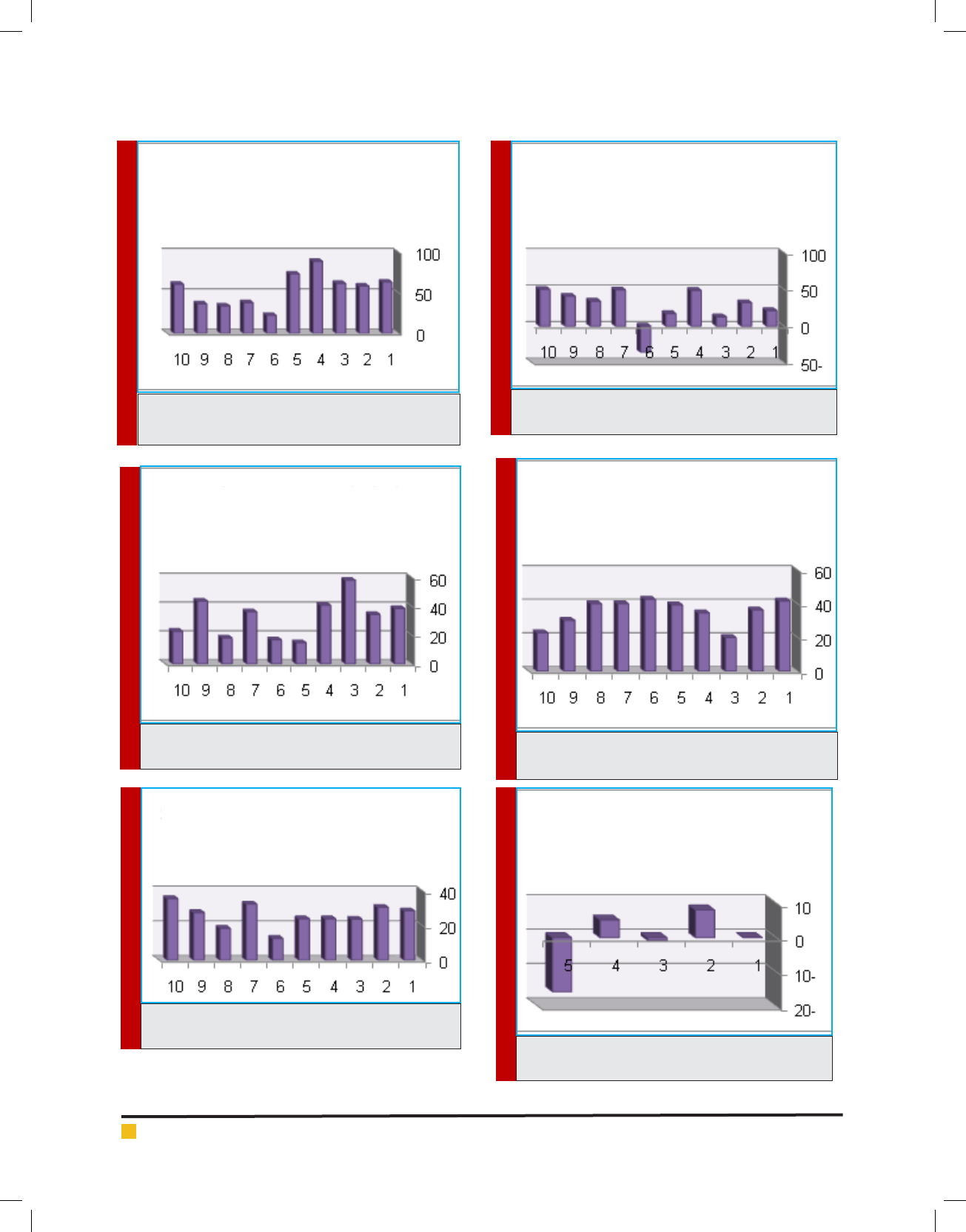
RESULTS AND DISCUSSION
In comparing 6 groups, maximum solubility is related
to 5/25% sodium hypochlorite and minimum solubility
is related to 0/2% chlorhexidine which is after control
group. After 5/25% sodium hypochlorite, percentage of
solubility is respectively related to chlorhexidine+ 2%
sodium dodecyl sulfate, chlorhexidine+ 4% benzalko-
niumchloride and 2/5% sodium hypochlorite.
In addition, descriptive statistic table for 6 groups is
as follow:
Statistical analysis of ANOVA with 95% as con dence
level was performed by 6 groups. And p<0/05 indiçâted
that there is no signi ant différence (P=0/0).
In addition, in Hemogeneity of variances test (P<0.05),
variance of 6 group, has signi cant difference (P=0.011).
For comparing average of 6 groups we used Welch
test in which signi cant difference between groups was
observed (P=.00).
For pairwise comparing of groups, Tamhane test was
used. Results indicated that there is signi cant differ-
ence between group 1 (5/25% sodium hypochlorite) with
group 6 (normal saline) and group 5 (0/2% chlorhex-
idine) group 3 (chlorhexidine+ benzalkoniumchloride)
with group 6, group 4 (sodium dodecyl sulfate) with
group 6 and group 5 with group 6. It means that nor-
mal saline and chlorhexidine has no ability of solving
organic tissue.
On the other hand, there is not signi cant difference
between group 1 with group 2,3 and 4. It means that
solubility of these groups is approximate to solubility of
5/25% sodium hypochlorite.
Root treatment without operation is predictable
method for tooth protection which is withdrawn in case
of no treatment (Johnson et al, 2008). Initial etiologic
factor in formation of pulp waste and priapical bac-
teria were studied (Kandaswamy and Venkateshbabu
2010; Guerreiro-Tanomaru et al, 2011; Martin 1991;
Mohammadi and Abbott 2009, Portenier et al, 2002).
Micro-organisms may be existed in root canal, dentinal
tubules, secondary canals and apical strait (Kandaswamy
and Venkateshbabu 2010;Baumgartner et al, 2007; Iqbal
2012). In some dentinal teeth, even DEJ was infected
(Zehnder et al, 2003).
If cleaning is not performed appropriately, necrosis
residuals of soft tissue is acting as feeding resource of
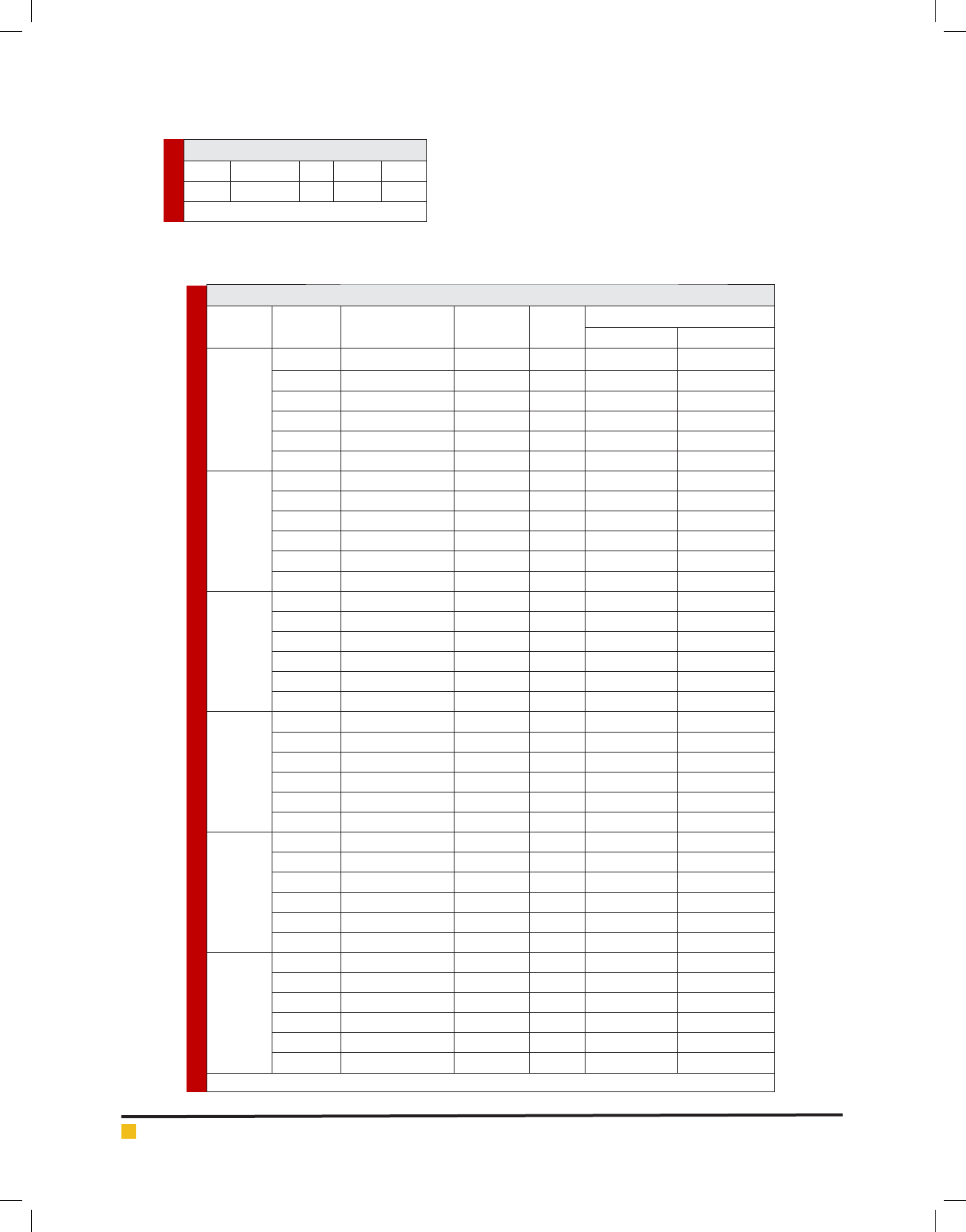
Table 1. solutions under experiment
Solution
code number
Solution name Sample
number
1NaOCl 25/5%10
2NaOCl 5/2%10
3BKC 4% +CHX 2/0%10
4SLS 2% +CHX 2/0%10
5CHX 2/0%10
6NaCl 9/0%5
Samira Shahsiah et al.
44 EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
DIAGRAM 1. Root dentine section which is covered
with smear layer resulted from canal working tools
DIAGRAM 2. Root dentine section which is covered
with smear layer resulted from canal working tools
DIAGRAM 3. Root dentine section which is covered
with smear layer resulted from canal working tools
DIAGRAM 4. Root dentine section which is covered
with smear layer resulted from canal working tools
DIAGRAM 5. Root dentine section which is covered
with smear layer resulted from canal working tools
DIAGRAM 6. Root dentine section which is covered
with smear layer resulted from canal working tools
study tissue solubility
of group 1
study tissue solubility
of group 2
study tissue solubility
of group 3
study tissue solubility
of group 4
study tissue solubility
of group 5
study tissue solubility
of group 6
Samira Shahsiah et al.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE 45
remained bacteria and can contaminate canal again
(Torabinejad , et al, 2003; Sassone et al, 2008; Hariharan
et al, 2010). Thus, rst and most important aim in endo-
dontic treatment is full elimination of microorganisms
from root canal system and providing an environment
for restoring per apical tissue Siqueira et al, 2009; Regan
and Fleury 2006). Achieving this goal is possible with
elimination of disease tissues and prevention from sec-
ond pollution until root canal space is converted into a
resource for infection (Rossi-Fedele et al, 2010; Vianna
et al, 2009). Mechanical use of tools cannot effectively
Table 2. average of tissue solubility
percentage of solutions under study
SOLUTION UNDER
STUDY
average of tissue
solubility
NaOCl 25/5%70/53%
NaOCl 5/2%07/27%
BKC4% CHX + 2/0%39/32%
SLS 2% CHX + 2/0%83/34%
CHX 2/0%61/25%
normal saline66/0-%
DIAGRAM 7. Root dentine section which is covered with smear layer resulted from canal working tools
Table 3. descriptive statistics
N Mean Std.
Deviation
Std. Error 95% Con dence Interval for Mean Minimum Maximum
Lower Bound Upper Bound
1 10 1.3470 .50193 .15872 .9879 1.7061 .57 2.20
2 10 .6710 .64264 .20322 .2113 1.1307 -.89 1.28
3 10 .8180 .34902 .11037 .5683 1.0677 .38 1.44
4 10 .8780 .20460 .06470 .7316 1.0244 .51 1.08
5 10 .6570 .17353 .05487 .5329 .7811 .31 .89
6 5 -.0180 .23221 .10385 -.3063 .2703 -.40 .20
Total 55 .7728 .50398 .06251 .6479 .8977 -.89 2.20
Table 4. ANOVA analysis
Sum of
Squares
df Mean
Square
F Sig.
Between Groups 6.918 6 1.153 7.161 .000
Within Groups 9.338 58 .161
Total 16.256 64
Table 5. HVariances analysis
Levene Statistic df1 df2 Sig.
3.085 6 58 .011
comparing percentage of tissue
solubility
Samira Shahsiah et al.
46 EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
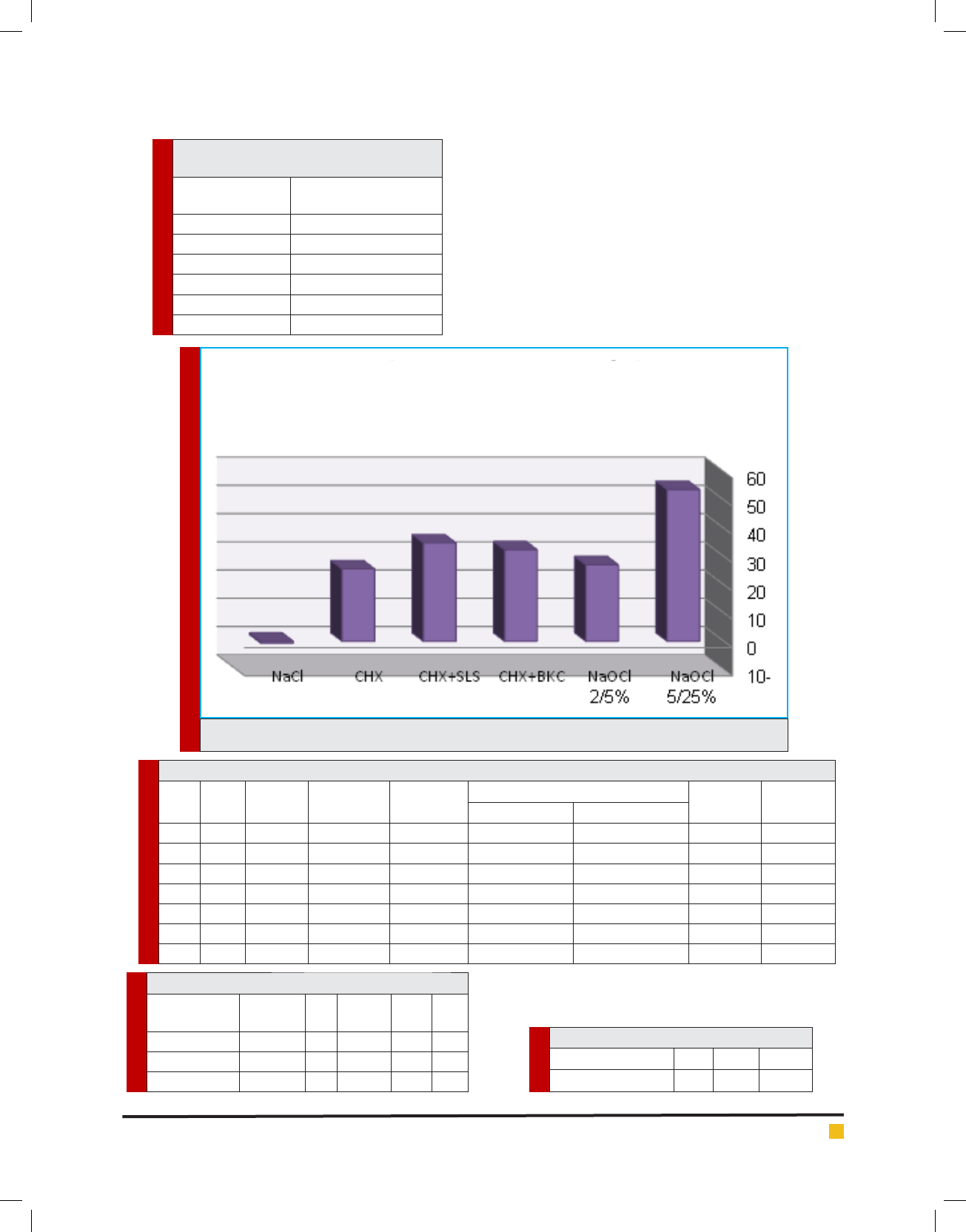
Table 6. Welch analysis
Statistica df1 df2 Sig.
Welch 10.749 6 23.054 .000
a. Asymptotically F distributed.
Table 7. Tamhane analysis
(I) group (J) gruop Mean Difference
(I-J)
Std. Error Sig. 95% Con dence Interval
Lower Bound Upper Bound
1
2 .67600 .25786 .315 -.2405 1.5925
3 .52900 .19333 .266 -.1650 1.2230
4 .46900 .17140 .320 -.1870 1.1250
5 .69000* .16794 .035 .0355 1.3445
6 1.36500* .18968 .000 .6542 2.0758
2
1 -.67600 .25786 .315 -1.5925 .2405
3 -.14700 .23126 1.000 -1.0011 .7071
4 -.20700 .21327 1.000 -1.0448 .6308
5 .01400 .21050 1.000 -.8244 .8524
6 .68900 .22822 .196 -.1756 1.5536
3
1 -.52900 .19333 .266 -1.2230 .1650
2 .14700 .23126 1.000 -.7071 1.0011
4 -.06000 .12794 1.000 -.5281 .4081
5 .16100 .12326 .994 -.2994 .6214
6 .83600* .15154 .003 .2517 1.4203
4
1 -.46900 .17140 .320 -1.1250 .1870
2 .20700 .21327 1.000 -.6308 1.0448
3 .06000 .12794 1.000 -.4081 .5281
5 .22100 .08484 .320 -.0790 .5210
6 .89600* .12235 .003 .3396 1.4524
5
1 -.69000* .16794 .035 -1.3445 -.0355
2 -.01400 .21050 1.000 -.8524 .8244
3 -.16100 .12326 .994 -.6214 .2994
4 -.22100 .08484 .320 -.5210 .0790
6 .67500* .11745 .021 .1043 1.2457
6
1 -1.36500* .18968 .000 -2.0758 -.6542
2 -.68900 .22822 .196 -1.5536 .1756
3 -.83600* .15154 .003 -1.4203 -.2517
4 -.89600* .12235 .003 -1.4524 -.3396
5 -.67500* .11745 .021 -1.2457 -.1043
*.The mean difference is signi cant at the 0.05 level.
clean complex tubular networks of canal (Mehrvar-
zfar and Saghiri 2011). So using detergents along with
mechanical preparation is needed (Tirali et al, 2013;
Torabinejad et al, 2003). These materials complete
mechanical debridementby ushing out debris, solving
necrosis tissues, removing smear layer, and disinfection
Samira Shahsiah et al.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE 47
of root canal system. There is no single solution that can
do all these (Rossi-Fedele, et al, 2012).
Our ai mis quantitative comparaison of tissue solu-
biity of NaOCl solutions and converted chlorhexidine.
Solution under-study in This resarci inclue NaOCl 25/5%,
NaOCl 5/2%, CHX2/0%, CHX+BKCandCHX+SLS. sodium
hypochlorite is mostly used in root treatment however
toxicityof this material for pri apical tissues is remained
as a basic concern (Cobankara et al, 2010). Chlorhexidine
was selected due to anti-microbial properties, less toxic-
ity than NaOCl, biocompatibility, and its stability of the
experiment. But it is proved that (Arcangelo, 2007) this
material has no acceptable capacity in high densities for
solving organic tissue so two type of surfactantswere
added ito CHX in order to increase solubility.
Results indicated that maximum solubility is related
to 5/25% sodium hypochlorite and average nega-
tive tissue solubility was related to normal saline.
After25/5%NaOCl, CHX+SLS had maximum tissue solu-
bility. Statistical analysis of ANOVA with 95% as con-
dence level was performed by 6 groups. And p<0/05
indicates that there is no signi ant différence (P=0/0).
In addition, in Hemogeneity of variances test (P<0.05),
variance of 6 group, has signi cant difference (P=0.011).
For comparing 6 group median, Welch test was used
in which signi cant difference was observed in groups
(P=0.0). for pairwise comparison of groups, Tamhane
was used. As there is no similar research in this case
we tested all solutions separately. In this study, average
solubility was related to NaOCl 25/5% and 5/2% which
was respectively 7/53% and 07/27% while there was no
signi cant difference in both group considering solubil-
ity (P=315). In addition, 25/5% NaOCl had maximum
tissue solubility. This case is compatible with Cobankara
et al (2010), Cbristensen et al (2008), Arcangelo et al
(2007), Naenni et al (2004), Okino et al (2004), Turkun
et al (1997), Hand et al (1998).
CONCLUSION
25/5% NaOCl had maximum tissue solubility. Other than
0/2% CHX and normal saline. Considering tissue solu-
bility, there is no signi cant difference in other solution
with NaOCl 25/5. Consequently, based on this research
using SLS 2% CHX+ 2/0% in canal washing can have
similar effect as NaOCl 25/5% regarding solubility.
REFERENCES
Arcangelo C, Di Nardo Di Maio F, Stracci N, Spoto G, Malag-
nino VA, Caputi S. (2007). Pulp-dissolving ability of several
endodontic irrigants: a spectrophotometric evaluation. Int JIP;
20(2): 381.
Aulton M, Taylor K. (2008). Aulton’s Pharmaceutics: The
Design and Manufacture of Medicines. Thed.537-540.
Baumgartner JC, Johal S, Marshall JG. (2007). Comparison of
the antimicrobial ef cacy of 1.3% NaOCl/biopure MTAD to
5.25% NaOCl/15% EDTA for root canal irrigation. JOE; 33(1):
47-51.
Beltz RE, Torabinejad M, pouresmail M. (2003). Quantitative
analysis of the solubilizing action of MTAD, sodium hypochlo-
rite, and EDTA on bovine pulp and dentin. J Endod; 29(5):
334-337.
Christensen CE, F. McNeal S, Eleazer P. (2008). Effect of Low-
ering the pH of Sodium Hypochlorite on Dissolving Tissue in
Vitro. JOE. Apr; 34(4):449-452.
Clarkson RM, Moule AJ, Podlich H, Kellaway R, Macfarlane R,
Lewis D, Rowell J. (2006). Dissolution of porcine incisor pulps
in sodium hypochlorite solutions of varying compositions and
concentrations. Aust Dent J. Sep;51(3):245-51.
Cobankara FK, Ozkan HB, Terlemez A. (2010). Comparison of
organic tissue dissolution capacities of sodoum hypochlorite
and chlorine dioxide. JOE; 36(2): 272-274.
Effendy I, I. Maibach H. (1995). Surfactants and experimen-
tal irritant contact dermatitis. Contact Dermatitis Oct; 33(4):
217–225.
E. Hand R, L. Smith M, W. Harrison J. (1998). Analysis of the
Effect of Dilution on theNecrotic Tissue Dissolution Property
ofSodium Hypochlorite. JOE Feb;4(2):60-64.
E. Vianna M, P. F. A. Gomes B. (2009). Efficacy of sodium
hypochlorite combined with chlorhexidine against Entero-
coccus faecalis in vitro. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod; 107:585-589.
Guerreiro-Tanomaru JM, Morgental RD, Faria-Junior NB, Ber-
bert FLCV, Tanomaru-Filho M. (2011). Antibacterial effective-
ness of Peracetic Acid and conventional endodontic irrigants.
Braz Dent J; 22(4): 285-287.
Ibusquiza PS, J.R. Herrera J, Vázquez-Sánchez D, Parada A,
L. Cabo M. (2012). A new and efficient method to obtain ben-
zalkonium chloride adapted cells of Listeria monocytogenes.
Journal of Microbiological Methods. 91:57-61.
Iqbal A. (2012). Antimicrobial Irrigants in the Endodontic
Therapy. International Journal of Health Sciences; 6(2): 153-
158.
Irala LE, Grazziotin-Soares R, Salles AA, Munari AZ, Munari
JS. (2010). Dissolution of bovine pulp tissue in solutions con-
sisting of varying NaOCl concentrations and combined with
EDTA. Braz Oral Res. Jul-Sep;24(3):271-6.
J. Kleier D, E. Averbach R, Mehdipour O. (2008). The Sodium
Hypochlorite Accident: Experience of Diplomates of the Amer-
ican Board of Endodontics. JOE Nov;34(11):1346-50.
Johnson W T, Noblett W C. (2008). Cleaning & shaping. In:
Torabinejad M, Torabinejad M. Principles & practice endodon-
tics. 4thed.287-315.
Kandaswamy D, Venkateshbabu N. (2010). Root canal irrigants.
J Conserv Dent; 13(4):256-264.

Samira Shahsiah et al.
48 EVALUATION OF TISSUE DISSOLUTION ABILITY OF MODIFIED CHLORHEXIDINE BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Karale R, Thakore A, Shetty VK. (2011). An evaluation of anti-
bacterial ef cacy of 3% sodium hypochlorite, high-frequency
alternating current and 2% chlorhexidine on Enterococcus far-
calis: An in vitro study. J Conserv Dent; 14:2-5.
Krithikadatta J, Indira R, Dorothykalyani AL. (2007). Disinfec-
tion of dentinal tubules with 2% chlorhexidine, 2% metronida-
zole, bioactive glass when compared with calcium hydroxide
as intracanal medicaments. JOE; 33(12): 1473-1476.
Lee HL, I. Maibach H. (1996). Sodium Lauryl Sulfate. Contact
Dermatitis Oct;35(4):257–267.
Marple B, Ronald P, Benninger M. (2004). Safety review of
benzalkonium chloride used as a preservative in intranasal
solutions: An overview of conflicting data and opinions. Oto-
laryngology–Head and Neck Surgery; 130(1):131-41.
Martin H. (1991). Cleanliness, disinfection, and sterilization of
the root canal. Curr Opin Dent. 1991 Dec;1(6):734-436.
Mohammadi Z, Abbott PV. (2009). The properties and appli-
cations of chlorhexidine in endodontics. Int Endod J.
Apr;42(4):288-302.
M. Sassone L, Fidel RAS, Murad CF, Fidel SR, Hirata Jr R.
(2008). Antimicrobial activity of sodium hypochlorite and
chlorhexidine by two different tests. Aust Endod J; 34: 19–24.
Naenni N, Thoma K, Zehnder M. (2004). Soft tissue dissolution
of currently used and potential endodontic irrigants. J Endod;
30(11):785-787.
Neppelberg E, Costea DE, Vintermyr OK, Johannessen AC.
(2007). Dual effects of sodium lauryl sulphate on human oral
epithelial structure. Experimental Dermatology. 16:574–579.
Okino LA, Siqueira EL, Santos M, Bombana AC, Figueiredo
JA. (2004). Dissolution of pulp tissue by aqueous solution of
chlorhexidine digloconate and chlorhexidine digloconate gel.
Int Endod J; 37(1): 38-41.
Parirokh M, Jalali S, Haghdoost AA, Abbott JV. (2012). Com-
parison of the Effect of Various Irrigants on Apically Extruded
Debris after Root Canal Preparation.JOE Feb;38(2): 196–
199.
Paudel K R, Jaiswal A, Parajuli U, Bajracharya M. (2011). Dif-
ferent pharmacological solutions in intracanal irrigation.
Nepal Med Coll J; 13(2): 111-114.
Portenier I, Haapasalo H, Ørstavik D, Yamauchi M, Haapasalo
M. (2002). Inactivation of the Antibacterial Activity of Iodine
Potassium Iodide and Chlorhexidine Digluconate Against Ente-
rococcus faecalis by Dentin, Dentin Matrix, Type-I Collagen,
and Heat-Killed Microbial Whole Cells. JOE. Sep; 28(9):634-
637.
Regan JD, Fleury A A. (2006). Irrigants in non-surgical endo-
dontic treatment. J Ir Dent Assoc. Autumn;52(2):84-92.
Rossi-Fedele G, Dog˘ ramac E J, Guastalli A R, Steier L, Poli
de Figueiredo J A. (2012). Antagonistic Interactions between
Sodium Hypochlorite, Chlorhexidine, EDTA, and Citric Acid.
JOE; 38(4): 426-431.
Saber S, Hashem A. (2011). Ef cacy of different nal irriga-
tion activation techniques on smear layer removal. JOE; 37(9):
1272-1275.
Sajadi tabassi S.A, Mamaghani sani D. (1996). Investigation
of the effects of ionic surfactants on biological membranes
using human erythrocytes as a model. Contact Dermatitis
Oct;35(4):253–256.
Siqueira J F, Rôças I N, Favier I A, Lima K C. (2009). Ef cacy of
Instrumentation Techniques and Irrigation Regimens in Reduc-
ing the Bacterial Population within Root Canals. JOE.; 27(7):
236-237.
TiraliR E, Bodur H, Sipahi B, Sungurtekin E. (2013). Evalua-
tion of the antimicrobial activities of chlorhexidine gluconate,
sodium hypochlorite and octenidine hydrochloride in vitro.
Aust Endod J; 39: 15–18.
Torabinejad M, Khademi A A, Babagoli J, Cho Y, Johnson W
B, Bozhilov K. (2003). A New Solution for the Removal of the
Smear Layer. JOE; 29(3): 170-175.
Turkun M, Cengiz T. (1997). The effect of sodium hypochlorite
and calcium hydroxide on tissue dissolution and root canal
cleanliness. Int Endod J; 30(5): 335.
VS Hariharan, B Nandlal, KT Srilatha. (2010). Ef cacy of vari-
ous root canal irrigants on removal of smear layer in the pri-
mary root canals after hand instrumentation: A scanning elec-
tron microscopy study. J Indian Soc Pedod Prev Dent; 26(4):
271-277.
Zehnder M. (2006). Root Canal Irrigants. JOE May;32(5):389-
98.
Zehnder M, Grawehr M, Grawehr G, Waltimo T. (2003). Tissue-
dissolution capacity and dentin-disinfecting potential of cal-
cium hydroxide mixed with irrigating solutions. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod; 96: 608-612.
Zhang C, Tezel U, Li K, Liu D, Ren R, Du J (2011). Evaluation
and modeling of benzalkonium chloride inhibition and biodeg-
radation in activated sludge. Water R esearch. 45: 1238-1246.